One of the first things I do with an insomnia patient, whether it’s in a 1:1 session or in my group program, is show them the 3P Model of Insomnia.
It’s super simple and impactful, and you can start using it in your practice as well.
Despite being foundational in behavioral sleep medicine, it often gets overlooked in medical training, which is a shame, because it explains exactly why insomnia becomes chronic, and why certain treatments work while others don’t.
The slide below visually shows how insomnia evolves from acute to chronic.
Let’s walk through how you can use this with patients.
The 3P model explained simply
The 3P model describes insomnia in terms of predisposing, precipitating, and perpetuating factors.
Predisposing factors are like dry kindling. Precipitating factors are the spark. Perpetuating factors are the oxygen that keeps the fire burning.
Even when the original spark is gone, the fire doesn’t go out if oxygen is still feeding it.
Here’s how that plays out clinically.
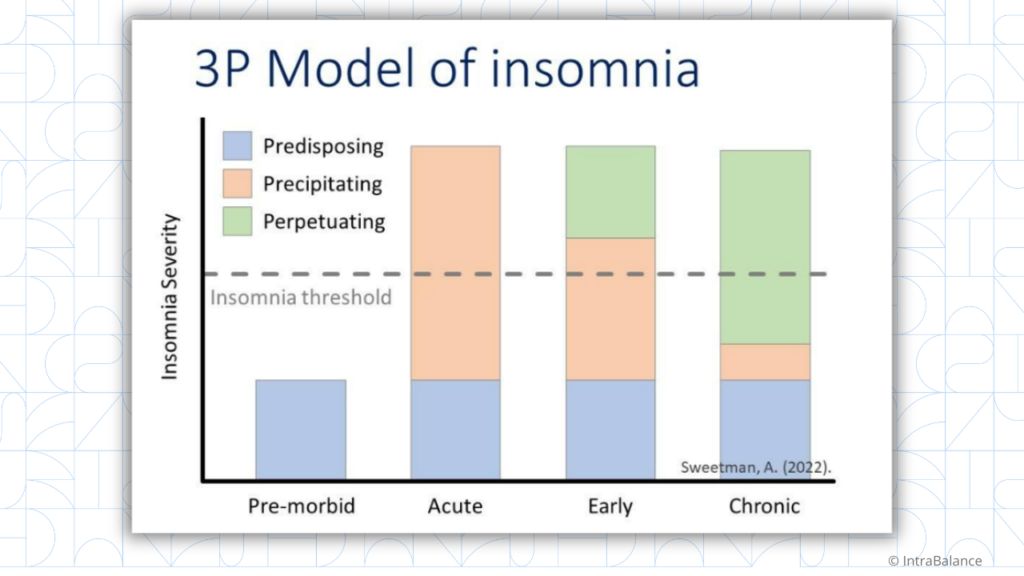
Predisposing factors increase vulnerability to insomnia but don’t cause it on their own.
Examples: Anxiety-prone or perfectionistic traits; female sex; advancing age; chronic medical or pain conditions, etc.
Precipitating factors are the events that trigger insomnia.
Examples: illness or injury; major life transitions; grief.
For many people, sleep normalizes once the stressor resolves. But for others, insomnia persists.
Perpetuating factors are the behaviors and cognitive processes that maintain insomnia after the original trigger is gone. This is the oxygen that keeps the fire burning.
Examples: Spending too much time in bed awake; Irregular sleep schedules; Conditioned arousal in the bedroom; Worrying about sleep or trying to force sleep; Rigid beliefs about “perfect” sleep; Cycling through different types of supplements or medications
Many of these behaviors feel adaptive and protective to patients, which is why they’re so easy to miss.
Why this model matters in clinical practice
When I go over the 3P model with patients, the idea is not to fixate on why their insomnia started, but to help them see how it’s being maintained.
The 3P model helps patients see that what matters now are the perpetuating factors, because they are the oxygen that’s keeping insomnia alive.
This reframing helps to get buy-in before you introduce behavioral changes.
CBT-I (cognitive behavioral therapy for insomnia) and ACT (acceptance and commitment therapy) work because they remove the oxygen that keeps the insomnia burning.
This also helps explain why medications may provide short-term relief, but often don’t lead to durable change when the perpetuating behaviors and cognitions remain intact.
How to frame this with your patients
You can say something like: “We don’t need to figure out what started your insomnia to help it improve. We’re focused on what’s keeping it going, because that’s what we can change.”
Framing it that way tends to reduce the fear and improve adherence to behavioral treatment.
If you’re working with patients struggling with chronic insomnia, this model can be a powerful starting point and help build rapport.
Save the slide and start using it in your practice…and let me know how it goes.
Next, collect your CME for this email below, using the Learner+ link.
If you missed last week’s video on how to use the Insomnia Severity Index (ISI), watch it here:
Did you learn something today? Click here to find out how Learner+ can help you meet your evolving educational goals. https://champions.learner.plus/?champion=Dr%20Nishi%20Bhopal
References:
Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008 Oct 15;4(5):487-504. PMID: 18853708; PMCID: PMC2576317.