
I’m writing this from Vancouver, BC, where I’m visiting family, and where the clocks just sprung forward for the last time:
BC has officially adopted permanent Daylight Saving Time.
As a sleep doctor, my first reaction was… complicated.
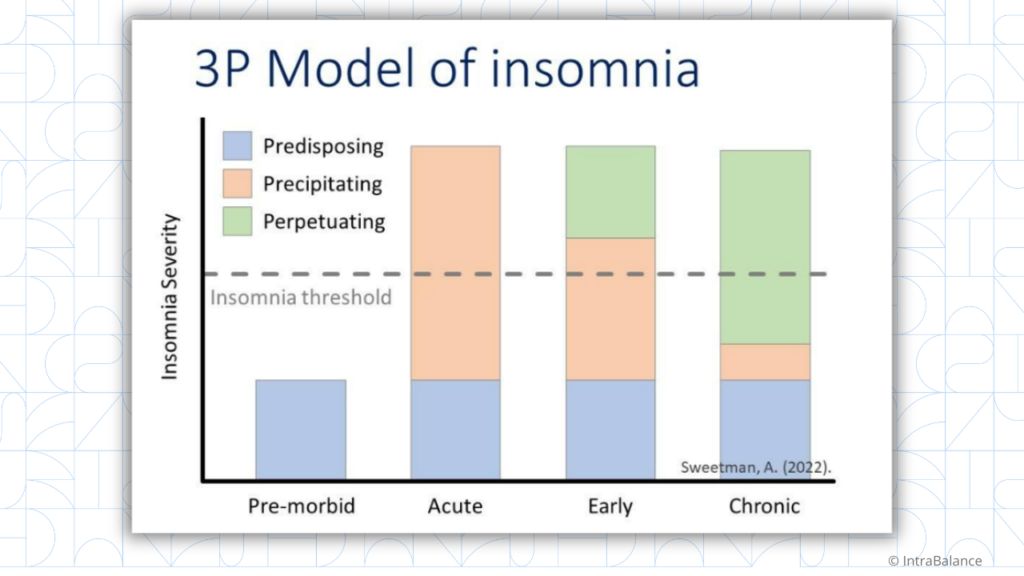
Sleep and circadian researchers (including the American Academy of Sleep Medicine) have been pushing to abolish the clock change for years.
But the recommendation has always been permanent Standard Time, not permanent DST.
Standard time is more aligned with our circadian biology. BC went in the other direction, driven by economics and public preference rather than scientific consensus.
So here we are.
While one hour might sound trivial, the spring transition is associated with a 6% increase in fatal car accidents, a 24% higher risk of heart attacks, an 8% increase in strokes, and an 11% rise in depressive episodes, all in the days following the switch.
Daylight Saving Time is a public health issue hiding in plain sight
So this is a good time to talk about ways to help your patients through it.
The Basics
The most important thing you can do is keep it simple. Behavioral interventions are the mainstay.. Some tips:
- Consistent wake times, even on weekends
- Plenty of bright light during the day, especially in the morning
- Avoiding alcohol, caffeine, and heavy meals late in the day
- Short 15–20 minute naps for a few days if patients are struggling
- Setting expectations:: “You might feel a little jet-lagged this week. It can take a couple of weeks to adjust..”
For patients on antidepressants
Chronotherapeutic adjuncts may enhance treatment response.
Evening chronotypes (your later-to-bed, later-to-rise patients) tend to struggle most with the spring transition. Morning bright light exposure (10,000 lux for 30 minutes) can help resynchronize their rhythms. Low-dose melatonin (0.5–5 mg) in the late afternoon or early evening can also support a phase advance, but timing should be individualized.
For cardiovascular patients
The spring transition carries the highest cardiovascular risk, so this population deserves a closer eye. The American Heart Association recommends optimizing circadian health through behavioral interventions rather than medication timing changes during DST.
Focus on consistent meal times, regular exercise, and morning light exposure to maintain circadian alignment.
For patients on sleep medications
Again, no dose adjustments are needed. Instead, use light and dark regulation to help patients adapt. Your evening chronotypes require more time to adjust to DST transitions and are most vulnerable to sleep disruption.
Who to watch most closely
Keep a closer eye this week on patients with mood disorders, cardiovascular disease, evening chronotypes, and anyone on medications with narrow therapeutic windows.
The good news: most people adjust within a week. The goal is just to make that week a little smoother.
If you want a ready-to-use system for managing sleep cases, not just the theory, but the actual clinical tools, The Clinical Sleep Kit is opening for enrollment again soon. Join the waitlist here.
Did you learn something today? Click here to find out how Learner+ can help you meet your evolving educational goals.
References:
(1) Permanent standard time is the optimal choice for health and safety: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2024 Jan 1;20(1):121-125. doi: 10.5664/jcsm.10898. PMID: 37904574; PMCID: PMC10758561.


Recent Comments